Managing obesity: a shared commitment
An essential resource that can help group plan sponsors better understand and manage the problem, and support their staff in managing this chronic and complex disease.
Download our white paper
The problem is real and is on the rise in the Canadian population. In 2022, 8.7 million adults reported being obese. In addition, some 10 million people said they were overweight.1
That’s a total of 18.7 million adult —three out of five— who said they carried excess weight that could have a negative impact on their health.
Obesity has been increasing in Canada for several decades and has even doubled since the 1970s. Globally, the prevalence of this condition has tripled since the 1950s, and it is estimated that nearly 2 billion people will suffer from it by 2030.2
What exactly are we talking about?
According to the Canadian Medical Association, obesity is a complex chronic disease.3 It is characterized by an abnormal or excessive accumulation of body fat that is harmful to health. Addressing it can generate tangible health benefits, but also economic benefits for organizations.
There are several ways of measuring excess fat, the most common one being the body mass index (BMI). The BMI is calculated by dividing the person’s weight by the square of their height, according to the following equation:4
BMI = weight(kg)/height(m)2
Health risk based on body mass index (BMI)
| Classification |
BMI class (kg/m2) |
Risk of problems |
| Normal weight |
18.5 – 24.9 |
Less |
| Excess weight |
25.0 – 29.9 |
More |
| Obesity, Class I |
30.0 – 34.9 |
High |
| Obesity, Class II |
35.0 – 39.9 |
Very high |
| Obesity, Class III |
>= 40.0 |
Extremely high |
However, although it is widely used as an indicator of the prevalence of the risk of one or more conditions associated with overweight developing, the BMI does not provide a complete picture of the situation and does not apply to the entire population.
To be relevant, the BMI must be assessed against other indicators. This is why specialists also consider waist circumference, for example, to identify the risks caused by overweight.
Other indicators that can more accurately reflect the risks associated with weight gain include blood tests, presence of persistent symptoms, lifestyle and eating habits, etc.
Health impacts
About 6.8% of deaths in Canada can be attributed to obesity.5 Therefore, weight and obesity issues are important to people’s health.
The condition is associated with several dozen types of complications, and the more excess weight, the greater the risk of mortality and the development of harmful conditions.
Also, people who are obese suffer many other effects on their mental and financial health, in addition to consequences in their social environment.
Obesity: Health consequences
| Gateway to many other diseases |
| Metabolic |
Mechanical |
Mental |
| Type 2 diabetes |
Sleep apnea |
Depression |
| Cardiovascular disease |
Knee osteoarthritis |
Anxiety |
| Cancer |
Chronic back pain |
|
 Decreased life expectancy
Decreased life expectancy Public health issue
Public health issue Worldwide
Worldwide
epidemic
Individual costs
In Canada, obesity generates an overall cost associated with short- and long-term disability and premature mortality of $1,943 per person per year.6 In the United States, obese people generate US$2,505 more in annual health costs than people whose weight is considered normal.7
Obesity also poses significant challenges for personal finances:
- Loss of income
- Associated mental health problems
- Drug costs
- Adaptation of equipment
- Etc.
People who are obese are 94% more likely to use health services.8 What’s more, their annual health care costs are higher than those of people of normal weight, ranging from 14.7% to 54%, depending on gender and country of residence.9
Obesity is a major risk factor for cardiovascular disease,10 but also for other health problems. The condition can also have a significant impact on people’s mental and financial health.11
The financial challenge for organizations
It is not surprising, therefore, that organizations that are concerned about the wellbeing of their staff want to provide them with the necessary resources and support.
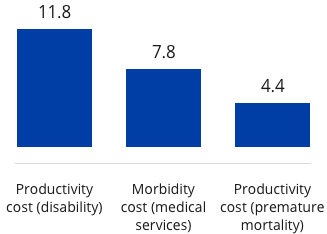
Prior to the COVID-19 pandemic in Canada, the total cost of lost productivity due to disability caused by obesity was $11.8 billion.12 These costs take into account absenteeism and presenteeism rates associated with obesity. In addition, $7.8 billion is attributable to the direct and indirect costs of various chronic diseases related to obesity.
Total annual cost of obesity in Canada, 2019
Broken down by type of cost, in $B
Source : Society of Actuaries Research Institute: Obesity Trends and the Impact on Morbidity and Mortality Costs, 2021.
For example, a person with Type 2 diabetes can cause up to $1,500 a year in lost productivity and absenteeism.13
Obesity can also have a significant impact on an organization’s financial health. People whose BMI indicates overweight up to obesity have significantly higher absenteeism rates than those with a normal BMI.
Depending on the job category and the magnitude of excess fat mass, absenteeism rates for obese individuals may be higher, ranging from 17% for white-collar workers to 37% for blue-collar workers. In addition, there are significant indirect labour productivity costs: for example, in the United States, some studies have estimated that organizations face between US$7,000 to $9,000 in additional costs due to obese employees compared to those who weigh less.14
In general, people with risk factors such as diabetes, high cholesterol, or high blood pressure report significantly lower productivity and higher medical expenses than people of normal weight with the same risk factors.15
A burden on group insurance plans
From 2019 to 2023,16 the total number of prescriptions for drugs used in obesity management increased by 82% a year in Canada, boosting the number of annual prescriptions from 250,000 in 2019 to 2.7 million in 2023, in part due to the greater availability of drugs.
This growth is also reflected in pharmaceutical costs and weight loss drugs represent an increasing share of private drug plans. From 2018 to 2024, the share of private drug plan costs for these drugs grew at a compounded annual growth rate of 24.8% according to the IQVIA™ Private Drug Plan Database. This represents an increase of 275%.
Share of weight-loss drug costs in private plan balance sheets

1 As of September 30, 2024
Source: IQVIA™ private drug plan database, 2024
For plan administrators, obesity poses a significant financial risk that is factored into plan pricing.17 The risk—and the premiums—increase in proportion to the degree of obesity, because of shorter life expectancies and the greater likelihood of disease of insured people.
Disability claims are also likely to grow for plans whose members face these issues.
As our disability portfolio illustrates, between 25 and 45 out of every 1,000 people covered by a group insurance plan applied for disability to deal with conditions generally related to obesity, such as stroke, coronary artery disease, diabetes, high blood pressure, etc.
Disability cases for obesity-related conditions
iA Financial Group, 2019-20241

1 As of Octobre 31, 2024
Proportion of disability cases for conditions generally related to obesity (diabetes, hypertension, malignant tumours of difestive system organs, arteriosclerosis, etc.) relative to all disability claims at iA Financial Group.
Source: iA Financial Group, 2024
Short-term disability (STD) claims to address conditions generally related to obesity make up about 3% of all disability claims in a given year. They grew by 20.3% from 2019 to 2024, with a compound annual growth rate of 3.8%.
Long-term disability (LTD) claims are approximately 4.5% of all claims. They increased by 10.3% over the same period, at a rate of 2% per year.
The solution lies in the workplace
Providing access to weight management resources and services can help people manage their weight more effectively and allow them to continue being productive members of the organization.
Obesity is a complex problem, and several factors contribute to it, including genetics, eating habits, the environment, physical activity, medication, sleep and stress.18, 19 To support obese people in the workplace, employers can offer insurance coverage that addresses all of these factors.
However, the issue is not solved by simply eating right, taking medication or being physically active. For example, obese people are often stigmatized, which can discourage them from seeking care.
Obesity is a complex, chronic condition influenced by multiple factors
Biological
The brain controls eating behaviour and appetite
Genetic
Approximately 40-70% of weight is linked to genetic inheritance
Psychological
Stress and psychological distress affect appetite
Medication
Several types of medication cause long-term weight gain
Environmental
Poor eating habits and a sedentary lifestyle increase risk
Social
Inequalities in socio-economic status and access to the healthcare system have an impact on weight gain
To ensure that an employee benefits program is able to help staff manage this condition, its administrators must clearly identify its causes and select the appropriate tools, programs and products accordingly. Indeed, obesity management must focus on improving overall health rather than just weight loss.20
Keys to a weight management program
Controlling obesity is not easy, particularly because access to treatment is difficult and resources are limited, including medications, weight management programs, and therapeutic support.21
Therefore, those struggling with obesity should have ongoing access to tools and services under their plan. Programs and support from specialists in nutrition, occupational therapy, physical activity, and other services such as cognitive behavioural therapy or pharmacotherapy, or even bariatric surgery, can sometimes be a solution to this complex issue.
Group plan administrators who choose to offer these products and services to cover more than the direct and immediate costs, such as drug expenditures, may lower long-term costs to the organization by reducing disability claims and absenteeism, and increasing employee engagement.
Such an integrated approach is all the more important because managing a single variable, for example by adopting an approach based only on drug therapy, may not generate sustainable results.22
The Canadian Medical Association, among other specialist organizations, proposes23 that an integrated weight management program ideally contains the following elements:
Elements of an organization’s weight management program
| Intervention |
Support from the plan administrator |
| Nutritional therapy: Personalized advice from specialists who focus on food choices. |
Coverage of the services of nutritionists, dieticians, etc. |
| Physical activity: Physical activity helps manage obesity and improves cardiovascular health and mental wellbeing. |
Coverage of fitness advisory services, such as kinesiologists, wellness account, etc. |
| Psychotherapeutic support: Cognitive-behavioural approaches to encourage the employees concerned to change their habits. |
Coverage of mental health programs and services (psychologist, psychotherapy, etc.); training in cognitive biases and stigmatization. |
| Drugs: To promote weight loss and the maintenance of a healthy weight. |
Coverage of drugs used to manage obesity. |
| Bariatric surgery: Need determined by the individual and specialists. |
Medical absence and return-to-work support policies. |
Compelling results
While the weight management journey may seem fraught with challenges, the gains can be significant for both employees and companies.
Weight loss improves conditions associated with overweight. For example, it only takes a modest weight loss to prevent the progression to type 2 diabetes. And even limited weight loss brings benefits. For example, a moderate decrease (5–10%) in fatty tissue is associated with reduced health care costs.24
In addition, weight loss in the order of 5–10% is also associated with lower blood pressure and HDL cholesterol levels, while for obese adults, weight loss can lead to a reduction in overall mortality of about 15%.25
In terms of overall health, small weight losses lead to significant improvements in several factors that can undermine cardiovascular health, such as glycemic and triglyceride levels. The improvements are even more significant when the weight loss is greater.
These improvements are possible when weight management is aimed at improving overall health, rather than simply percent weight loss.
Sources
1 Body mass index, overweight or obese, self-reported corrected, adult, by age group (18 years and older) | Statistics Canada
2 Update on the Obesity Epidemic: After the Sudden Rise, Is the Upward Trajectory Beginning to Flatten? | Current Obesity Reports
3 Obesity in adults: a clinical practice guideline | Journal of the Canadian Medical Association
4 Body Mass Index (BMI) Nomogram | Canada.ca
5 Percentage of deaths attributed to obesity in select countries worldwide in 2021: Statista
6 Obesity Trends and the Impact on Morbidity and Mortality Costs
7 New Weight Loss Drugs Expensive For Insurers to Cover, But May Help Address Costs of Obesity | Morningstar DBRS
8 Les conséquences économiques associées à l'obésité et l'embonpoint au Québec : les coûts liés à la consommation de médicaments et à l'invalidité - Mise à jour 2016 | Institut national de santé publique du Québec (In French only)
9 Le fardeau économique de l'obésité et de l'embonpoint : revue de la littérature |INSPQ.QC.CA (In French only)
10 Facteurs de risque | Institut de cardiologie de Montréal (In French only)
11 Report Card on Access to Obesity Care - Obesity Canada
12 Society of Actuaries Research Institute: Obesity Trends and the Impact on Morbidity and Mortality Costs, 2021
13 Reducing the Risk of Type 2 Diabetes Through Workplace Programs - Diabetes Canada
14 Kudel I, Huang JC, Ganguly R. Impact of Obesity on Work Productivity in Different US Occupations: Analysis of the National Health and Wellness Survey 2014 to 2015. J Occup Environ Med. 2018 Jan;60(1):6-11.
15 Sanchez Bustillos A, Vargas KG 3rd, Gomero-Cuadra R. Work productivity among adults with varied Body Mass Index: Results from a Canadian population-based survey. J Epidemiol Glob Health. 2015 Jun;5(2):191-9.
16 Medication Treatments for Diabetes and Obesity in Canada| IQVIA
17 New Weight Loss Drugs Expensive For Insurers to Cover, But May Help Address Costs of Obesity | Morningstar DBRS
18 Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report | National Institutes of Health
19 Badman MK, Flier JS. The gut and energy balance: visceral allies in the obesity wars. Science. 2005 Mar 25;307(5717):1909-14
20 Obesity in adults: a clinical practice guideline | Journal of the Canadian Medical Association
21 Report Card on Access to Obesity Care - Obesity Canada
22 Real-World Analysis of Glucagon Like Peptide-1 (GLP-1) Agonist Obesity Treatment Year-Two Clinical and Cost Outcomes. 2024.
23 Obesity in adults: a clinical practice guideline | Canadian Medical Association Journal
24 Ryan DH, Yockey SR. Weight Loss and Improvement in Comorbidity: Differences at 5%, 10%, 15%, and Over. Curr Obes Rep. 2017 Jun;6(2):187-194.
25 Kritchevsky SB, Beavers KM, Miller ME, Shea MK, Houston DK, Kitzman DW, Nicklas BJ. Intentional weight loss and all-cause mortality: a meta-analysis of randomized clinical trials. PLoS One. 2015 Mar 20;10(3):e0121993.